En klynge hvide telte i det østlige Sierra Leone er et af de steder, hvor læger, sygeplejersker og Røde Kors-frivillige arbejder på højtryk i et forsøg på at bremse den dødelige ebola-smitte.
KENEMA, 14 October 2014 (IRIN): We’re heading to the International Federation of the Red Cross (IFRC) Ebola treatment centre 15km out of Kenema town in eastern Sierra Leone.
It’s known locally as the “Ebola camp” because it’s made up of a dozen or so white tented structures set up outside. It is surrounded by lush green forest and mountains loom in the distance.
Day shift staff arrive at 8am in a minibus, exchanging greetings, making jokes.
Roughly 80 staff work here with an on-shift 2:1 staff-patient ratio.
They include Ministry of Health nurses; government social workers; international nurses; members of the water and sanitation, body removal and burial teams; cooks; laundry staff; administrators and logisticians.
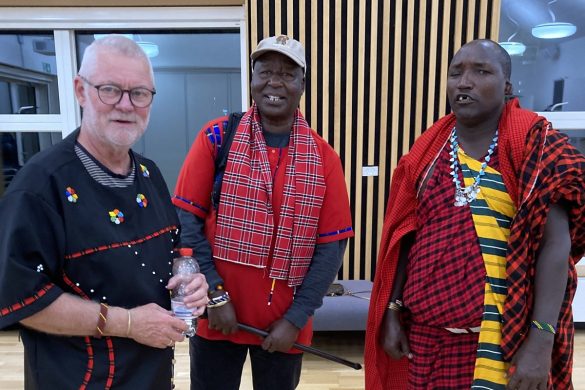
Many staff are Red Cross volunteers from Sierra Leone as well as Norway and Spain, following national appeals.
No clinical care to give
In the month since it opened, the centre has admitted 52 patients, discharging 13 thus far and burying 22. The Red Cross wants to scale up from 30 beds to 60 in the coming weeks, but needs more staff to do so.
The day we are there the centre is holding 15 confirmed patients – one suspected, one probable, and one man dies over the course of the day.
It is the first time IFRC is running an Ebola treatment centre. MSF trained them on every step of the process.
Leading the operation is a Spanish doctor, Marte Trayner Euxens, an emergency health specialist and long-time Red Cross volunteer, more used to doctoring following earthquakes or typhoons.
“The biggest challenge here is that you’re responsible for your team’s security. You can never let your guard down, and you have to be very conscious of everything around you at all times,” she told us.
The other challenge for a doctor is that there is no clinical care to give: just palliative medicine – oral rehydration solution, painkillers, anti-malarials and antibiotics.
They do not even give IV drips as they would pose an added danger to staff.
“It is more of a nursing job,” she said. But she is happy to be here and her medical family supports her decision.
“Patients have dignity and we humanitarians here need to help preserve it. I enjoy this work,” she said.
You may live
It is hard seeing so many patients die, says health worker Ibrahima Kemokai, but he is used to working with people in distress having nursed people through the latter part of the civil war in Sierra Leone.
“This is a very stressful disease to get, and you have to encourage people by telling them: you’re not the person with it, if you rest, you might get better. You have to change their mindset.”
Jestina Boyle, a government social worker working with patients, tells IRIN:
“I try to tell people to relax, to take their medication, to remain calm, to follow the rules and eat and sleep well… I tell them: you may not die here – you may live.”
Merete Benestad, a volunteer nurse from Norway is on her first day in the job. “I decided to come and then I had second thoughts, especially because my colleagues were questioning my decision. I researched it a lot and in the end I said `yes’ without fear,” she said.
Læs mere og se fotos og video hos IRIN News