Mange af Liberias ca. 30.000 hiv-patienter lades i stikken, mens ebola-smitten raser i landet. Knap en tredjedel af klinikkerne er lukket, og mange hiv-patienter bliver afvist eller er utrygge ved at bruge de klinikker, der stadig er åbne.
MONROVIA/DAKAR, 21 November 2014 (IRIN): Ebola has crippled the provision of treatment and care to people living with HIV/AIDS in Liberia, according to health workers and patients.
“We cannot get treatment normally now because of the outbreak of the Ebola disease in Liberia,” said 36-year-old Jeff Thompson, from Monrovia’s Jallah Town, who was diagnosed with HIV in 2011.
“Our care centres are closed and all the health workers are scared to come to work.”
There are an estimated 30,000 people living with HIV in Liberia, according to UNAIDS.
Before the Ebola outbreak, more than 70 percent of them had access treatment via 144 HIV/AIDS care centres scattered across the country.
But now, due to a shortage of health workers and fear about Ebola transmission, more than 60 percent these facilities have shut their doors, according to the National AIDS Control Program (NACP)
“My condition is getting worse by the day,” a 43-year-old HIV-positive woman in Monrovia, who declined to be named, told IRIN.
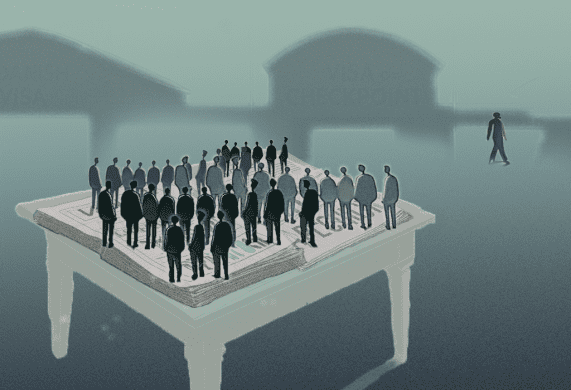
“I used to get treatment at the [St. Joseph’s] Catholic Hospital, but the place is closed down and now there is no way to get treatment. I think we [HIV/AIDS patients] have been forgotten.”
Home-based care
To help ensure uninterrupted care, save lives and prevent new infections, NACP says they are now going door-to-door in Montserrado County to either deliver antiretroviral drugs each week or else refer people to mobile treatment centres to fill prescriptions.
“We have launched an outreach programme. because if we don’t go out to them then we will be having a disaster,” said Sonpon Blamo Sieh, who heads the NACP.
“Our focus is to avoid reinfection and treatment failure leading to death. We made a lot of gains [in HIV/AIDS treatment access over the past 10 years], but if we are not mindful of the gains, we will be dragged down again.”
AAF has also been going door-to-door offering psychosocial and counselling services to people living with HIV/AIDS, making sure they take their drugs on time and trying to identify new patients.
“Our door-to-door treatment care is going very well,” Sieh said.
“Right now we are reaching hundreds of our people who were taking treatment at the care centres.”
Disrupted services
While some HIV services are still offered at operational general health facilities, many people say they don’t know where to go or when such treatment services will be available at which clinics.
“Right now, some of them want to give up because the normal centres for treatment are not open,” said Koffa Morris, director of the Anti-AIDS Foundation (AAF) in Monrovia. “But we tell them not to give up.”
For those who do still have access to HIV care services, some are too afraid to enter a hospital or clinic for fear of catching Ebola.
Others report being turned away by health workers who mistake them as suspected Ebola cases.
“In terms of diagnosis, the similarity and the conditions in question, Ebola comes with fever, rashes and red eyes, just like HIV,” Sieh said.
“And some of the health workers at the existing facilities are afraid to treat the patients because of the lack of Personal Protective Equipment materials at the centre.”
Sieh said that denying care to people with HIV/AIDS or disrupting their treatment not only negatively affects their health, but can lead to drug resistance.
“Treatment failure is quite dangerous,” he said.
“And when it comes to resistance for HIV, what that means is all of those patients will now get on with maybe second-line drugs, which are most costly.”
There is also a risk that Liberia could see an increase in the number of HIV cases if care facilities are not functioning.
“The idea is that many people will not be identified who [could] be HIV positive [and this] will lead to a multiplication of new cases,” he said.
“That is a serious problem.”
An imperfect solution
Due to financial constraints, the outreach programme, which is both time and labour intensive, currently only targets people living in Montserrado County.
“Unfortunately, the home treatment programmes have been hit with a lack of funds,” Sieh said.
“This is a serious bottleneck to the programme.”
While many patients have welcomed the door-to-door service, they say there are also many challenges.
“I appreciate this new way,” said Marlene*, a 45-year-old woman who has been living with HIV since 2009.
“But the only thing I don’t like about the house treatment is that other people get to know you are HIV-positive. However, something is better than nothing.”
The care centre she used to frequent also offered treatment for malaria, tuberculosis and other diseases, so no one could tell what you entered the clinic for, she explained.
Other patients complain about missed appointments from the door-to-door service and late drug deliveries.
“I think they are grabbing the idea [of home-based care],” AAF’s Morris said.
“The only thing is that most of the times their drugs are not on time. There is often a delay in getting the drugs to the people due to a lack of logistics and other funding, which are needed to speed up the exercise.”
Health concerns
Health workers have also raised concerns about mother-to-child transmission, now that more women are giving birth at home because home-based HIV care services aren’t available to pregnant women.
NACP says it is working with the Ministry of Health and donors to expand the programme nationwide. They are also working “around the clock” to reopen some of the closed centres.
But for many, it may already be too late.
“His situation is terrible,” said Matthew Sampson, the father of an 18-year-old with HIV. “Since the Ebola outbreak began, he has been forgotten. [There is] no hospital to take [him to for] treatment. They need to focus on them too,” he told IRIN.
“My son is dying slowly.”
*Not a real name