GENEVA, 9 May 2015 (WHO): Today WHO declares Liberia free of Ebola virus transmission. Forty-two days have passed since the last laboratory-confirmed case was buried on 28 March 2015. The outbreak of Ebola virus disease in Liberia is over.
Interruption of transmission is a monumental achievement for a country that reported the highest number of deaths (4.716, red.) in the largest, longest, and most complex outbreak since Ebola first emerged in 1976. At the peak of transmission, which occurred during August and September 2014, the country was reporting from 300 to 400 new cases every week.
During those 2 months, the capital city Monrovia was the setting for some of the most tragic scenes from West Africa’s outbreak: gates locked at overflowing treatment centres, patients dying on the hospital grounds, and bodies that were sometimes not collected for days.
Flights were cancelled. Fuel and food ran low. Schools, businesses, borders, markets, and most health facilities were closed. Fear and uncertainty about the future, for families, communities, and the country and its economy, dominated the national mood.
Tilfælde i alle landets regioner
Though the capital city was hardest hit, every one of Liberia’s 15 counties eventually reported cases. At one point, virtually no treatment beds for Ebola patients were available anywhere in the country. With infectious cases and corpses remaining in homes and communities, almost guaranteeing further infections, some expressed concern that the virus might become endemic in Liberia, adding another – and especially severe – permanent threat to health.
It is a tribute to the government and people of Liberia that determination to defeat Ebola never wavered, courage never faltered. Doctors and nurses continued to treat patients, even when supplies of personal protective equipment and training in its safe use were inadequate. Altogether, 375 health workers were infected and 189 lost their lives.
Local volunteers, who worked in treatment centres, on burial teams, or as ambulance drivers, were driven by a sense of community responsibility and patriotic duty to end Ebola and bring hope back to the country’s people. As the number of cases grew exponentially, international assistance began to pour in. All these efforts helped push the number of cases down to zero.
Sidste patient døde 27. marts
Liberia’s last case was a woman in the greater Monrovia area who developed symptoms on 20 March and died on 27 March. The source of her infection remains under investigation. The 332 people who may have been exposed to the patient were identified and closely monitored. No one developed symptoms; all have been released from surveillance.
Health officials have maintained a high level of vigilance for new cases. During April, the country’s 5 dedicated Ebola laboratories tested around 300 samples every week. All test results were negative.
Fortsat risiko for spredning fra Guinea og Sierra Leone
While WHO is confident that Liberia has interrupted transmission, outbreaks persist in neighbouring Guinea and Sierra Leone, creating a high risk that infected people may cross into Liberia over the region’s exceptionally porous borders.
The government is fully aware of the need to remain on high alert and has the experience, capacity, and support from international partners to do so. WHO will maintain an enhanced staff presence in Liberia until the end of the year as the response transitions from outbreak control, to vigilance for imported cases, to the recovery of essential health services.
Udbruddet begyndte langsomt
The start of the outbreak was deceptively slow. Health officials were on high alert for cases following WHO’s confirmation, on 23 March 2014, of the Ebola outbreak in Guinea. Liberia’s first 2 cases, in the northern county of Lofa near the border with Guinea, were confirmed on 30 March 2014.
On 7 April, 5 more cases were confirmed, 4 in Lofa and 1 in Monrovia. All 5 died. The situation then stabilized, with no new cases reported during April and most of May.
Further cases were detected in early June, mainly in Lofa county, but the trend did not look alarming, especially when compared with the situation elsewhere. At the end of June, Liberia reported 41 cases, compared with 390 in Guinea and 158 in Sierra Leone.
The impression of a calm situation turned out to be an illusion. The first additional cases in Monrovia were reported in mid-June. The city was ill-prepared to cope with the onslaught of infections that rapidly followed as the virus raced through hospitals, communities, and eventually entire neighbourhoods.
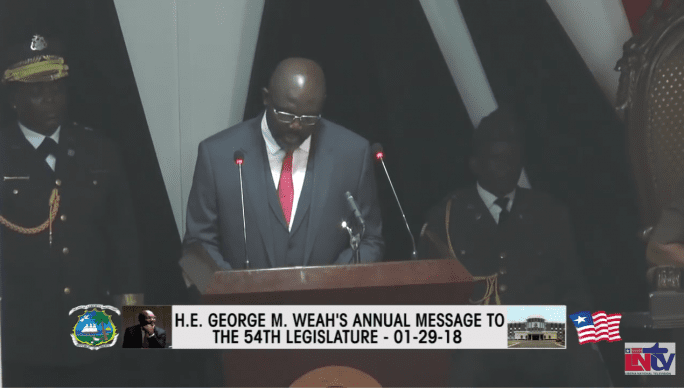
Præsidenten erklærede undtagelsestilstand
Case numbers that had multiplied quickly began to grow exponentially. On 6 August, President Ellen Johnson Sirleaf declared a three-month state of emergency and announced several strict measures aimed at getting cases down.
In mid-August, a WHO team of emergency experts estimated that Monrovia needed 1000 beds just to treat currently infected patients. Only 240 beds were available.
In September, WHO began construction of a new treatment centre, using teams of 100 construction workers labouring in round-the-clock shifts. On 21 September, the Island Clinic was formally handed over by WHO to Liberia’s Ministry of Health and Social Welfare. The clinic added 150 beds to Monrovia’s limited treatment capacity. However, within 24 hours after opening, the clinic was overflowing with patients, demonstrating the desperate need for more treatment beds.
WHO supported the construction of 2 additional Ebola treatment centres, augmenting Monrovia’s treatment capacity by another 400 beds. The remaining need was eventually met by multiple partners. The rapid increase in treatment capacity, especially in Monrovia, likely did much to turn the outbreak around.
Antallet af overlevere voksede
The outbreak began to subside in late October, when more new cases were detected early and rapidly treated in isolation, and more safe and dignified burials were performed. Case-fatality rates dropped. As the number of survivors grew, public perceptions changed from viewing treatments centres as “death traps” to seeing them as places of hope. That altered perception, in turn, encouraged more patients to seek early treatment.
The incidence of new cases stabilized in mid-November, with daily reports showing only 10 to 20 new cases. During the early months of 2015, cases dwindled further, eventually allowing detection and investigation of the last remaining chains of transmission. From late March on, daily reports consistently showed zero cases.
En trussel mod landets økonomi og sammenhængskraft
The first decisive factor was the leadership shown by President Sirleaf, who regarded the disease as a threat to the nation’s “economic and social fabric” and made the response a priority for multiple branches of government. Her swift and sometimes tough decisions, frequent public communications, and presence at outbreak sites were expressions of this leadership.
As President Sirleaf famously stated in her memoir, “The size of your dreams must always exceed your current capacity to achieve them. If your dreams do not scare you, they are not big enough.”
Second, health officials and their partners were quick to recognize the importance of community engagement. Health teams understood that community leadership brings with it well-defined social structures, with clear lines of credible authority. Teams worked hard to win support from village chiefs, religious leaders, women’s associations, and youth groups.
One of the first signs that the outbreak might be turned around appeared in September 2014, when cases in Lofa county, Ebola’s initial epicentre, began to decline after a peak of more than 150 cases a week in mid-August. Epidemiologists would later link that decline to a package of interventions, with community engagement playing a critical role.
In Lofa, staff from the WHO country office moved from village to village, challenging chiefs and religious leaders to take charge of the response. Community task forces were formed to create house-to-house awareness, report suspected cases, call health teams for support, and conduct contact tracing.
Gennemsigtige vægge i behandlingscentre
See-through walls around the treatment centre replaced opaque ones, allowing families and friends to watch what was happening inside, thus dispelling many rumours. Calls for transportation to treatment facilities or for burial teams were answered quickly, building confidence that teams were there to help.
The effectiveness of this response, which was duplicated elsewhere, points to a third factor: generous support from the international community, including financial, logistical, and human resources. This support added more treatment beds, increased laboratory capacity, and augmented the number of contact tracing and burial teams. The deployment of self-sufficient foreign medical teams from several countries had a dramatic impact on the outbreak’s evolution.
Finally, strong coordination of the international and national response was essential for success. International support was slow to start, but abundant when it arrived. Innovations such as the Presidential Advisory Committee on Ebola and introduction of a incident management system helped ensure that resources and capacities were placed where needed.
Many of these lessons and experiences are reflected in WHO’s new response plan, which aims to identify all remaining cases in West Africa by June 2015.