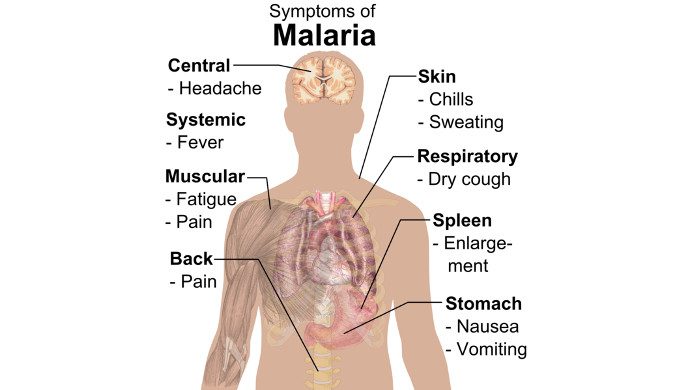
Om malaria

Halvdelen af jordens befolkning er i risiko for at få malaria. Man skønner, at der hvert år er over 200 millioner tilfælde af malaria i verden, og at omkring 660.000 mennesker dør af sygdommen.
Malaria findes især i de afrikanske lande syd for Sahara, hvor 90 procent af alle tilfælde forekommer. Her er det især børn under fem år, der bliver smittet, og tusindvis af børn under fem år dør hvert år på grund af malaria.
Kilde: Læger uden Grænser
GENEVA, 17 November 2016 (WHO): The world’s first malaria vaccine will be rolled out in pilot projects in sub-Saharan Africa, WHO confirmed today. Funding is now secured for the initial phase of the programme and vaccinations are due to begin in 2018.
The vaccine, known as RTS,S, acts against P. falciparum, the most deadly malaria parasite globally, and the most prevalent in Africa. Advanced clinical trials have shown RTS,S to provide partial protection against malaria in young children.
“The pilot deployment of this first-generation vaccine marks a milestone in the fight against malaria,” said Dr Pedro Alonso, Director of the WHO Global Malaria Programme. “These pilot projects will provide the evidence we need from real-life settings to make informed decisions on whether to deploy the vaccine on a wide scale.”
Vaccine financing and development
The Global Fund to Fight AIDS, Tuberculosis and Malaria today approved US$ 15 million for the malaria vaccine pilots, assuring full funding for the first phase of the programme. Earlier this year, Gavi, the Vaccine Alliance and UNITAID announced commitments of up to US$ 27.5 million and US$ 9.6 million, respectively, for the first 4 years of the vaccine programme.
RTS,S was developed through a partnership between GlaxoSmithKline and the PATH Malaria Vaccine Initiative (MVI), with support from the Bill & Melinda Gates Foundation and from a network of African research centres.
“WHO recognizes and commends the leadership and support of all funding agencies and partners who have made this achievement possible,” said Dr Jean-Marie Okwo-Bele, Director of the WHO Department of Immunization, Vaccines and Biologicals.
Vaccine programme recommended by two WHO advisory bodies
In October 2015, two independent WHO advisory groups comprised of the world’s foremost experts on vaccines and malaria – the Strategic Advisory Group of Experts (SAGE) on Immunization and the Malaria Policy Advisory Committee (MPAC) – recommended pilot implementation of the RTS,S vaccine in 3 to 5 settings in sub-Saharan Africa. These recommendations followed a July 2015 announcement that the European Medicines Agency (EMA) had issued a positive scientific opinion of the RTS,S vaccine.
WHO officially adopted the SAGE-MPAC recommendations in January 2016 and has since worked to mobilize financial support for the pilots and to finalize the programme design. The pilot programme will evaluate the feasibility of delivering the required 4 doses of RTS,S; the impact of RTS,S on lives saved; and the safety of the vaccine in the context of routine use.* It will also assess the extent to which the vaccine’s protective effect demonstrated in children aged 5–17 months old in the Phase 3 trial can be replicated in real-life settings.
Country selection
RTS,S is the first malaria vaccine to successfully complete pivotal Phase 3 testing. The Phase 3 trial enrolled more than 15,000 infants and young children in 7 countries in sub-Saharan Africa. Countries that participated in the Phase 3 clinical trials will be prioritized for inclusion in the WHO pilot programme. Consultations are ongoing and the names of the 3 selected countries will be announced in the coming weeks.
A complementary control tool
The RTS,S vaccine is proposed as a tool to complement the existing package of WHO-recommended malaria preventive, diagnostic and treatment measures and will be used in combination with the current interventions. Other tools include: long-lasting insecticidal bed-nets, spraying inside walls of dwellings with insecticides, preventive treatment for infants and during pregnancy, prompt diagnostic testing, and treatment of confirmed cases with effective anti-malarial medicines.
Deployment of these tools has already dramatically lowered malaria disease burden in many African settings. Between 2000 and 2015, the rate of new malaria cases in sub-Saharan Africa fell by 42% and malaria mortality rates fell by 66%. However, this region continues to account for approximately 90% of global malaria cases and deaths.
As RTS,S is only partially effective, it will be essential that any vaccinated patients with a fever be tested for malaria, and that all those with a confirmed malaria diagnosis are treated with high quality, effective anti-malarial medicines.
Target groups
There were 2 target age groups in the Phase 3 RTS,S trials:
- Infants who received the malaria vaccine together with other routine childhood vaccines at 6, 10 and 14 weeks of age.
- Older children who received their first dose of the malaria vaccine between 5 and 17 months of age.
Among children in the older age group, there was a risk of febrile seizures within 7 days after any of the vaccine doses. Among infants, this risk was only apparent after the fourth dose. There were no long-lasting consequences due to any of the febrile seizures.
Among children in the older age group, an increase in the number of cases of meningitis and cerebral malaria was found in the group receiving the malaria vaccine compared to the control group. The significance of these findings in relation to the vaccination is unclear. An excess of meningitis and cerebral malaria was not seen in infants aged 6–12 weeks.